In the world of prostate cancer screening, there has long been a debate surrounding the necessity of a digital rectal exam (DRE). While some argue that this physical examination is essential in detecting potential abnormalities, others question its effectiveness and raise concerns about patient discomfort. With advancements in technology and alternative screening methods available, it is worth exploring whether the DRE is truly necessary or if it is time to reassess our approach to prostate cancer screening.
Understanding Prostate Cancer
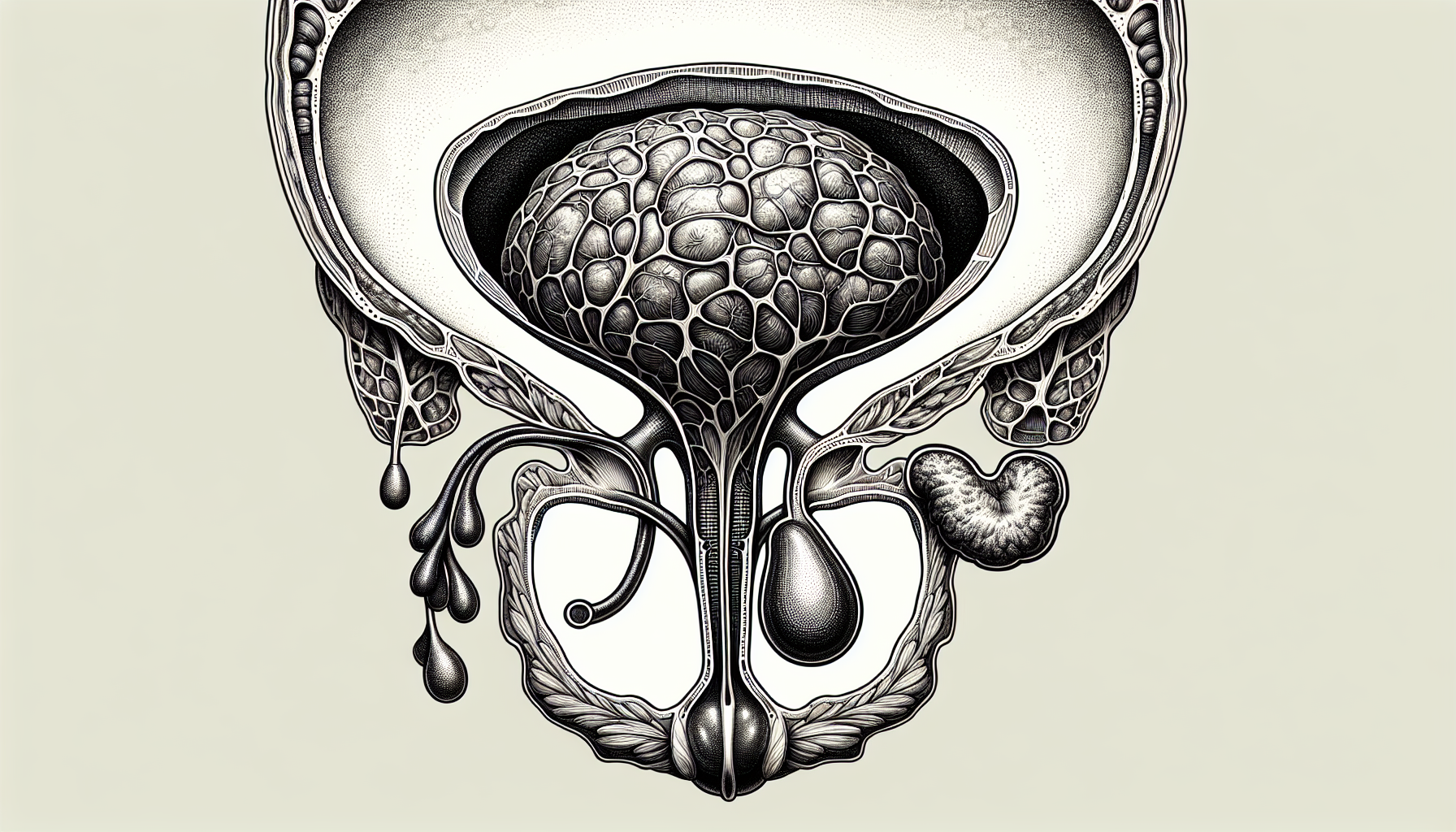
Overview of prostate cancer
Prostate cancer is a type of cancer that develops in the prostate gland, a small walnut-shaped gland located just below the bladder in men. It is the second most common cancer in men worldwide, with approximately 1.3 million new cases diagnosed each year. Prostate cancer occurs when abnormal cells in the prostate gland multiply and form a tumor. If left untreated, it can spread to other parts of the body.
Prevalence and statistics
Prostate cancer predominantly affects older men, with the average age at diagnosis being around 66. It is more common among African-American men and those with a family history of the disease. According to the American Cancer Society, about 1 in every 8 men will be diagnosed with prostate cancer in their lifetime. However, the survival rate is generally high, with over 98% of men being alive 5 years after diagnosis.
Risk factors associated with prostate cancer
Several risk factors have been identified for prostate cancer, including age, family history, race, and certain genetic mutations. Age is the most significant risk factor, as the likelihood of developing prostate cancer increases with age. Having a family history of prostate cancer, especially in a first-degree relative, such as a father or brother, also increases the risk. African-American men have a higher incidence and mortality rate from prostate cancer compared to other racial or ethnic groups. Additionally, certain gene mutations, such as the BRCA1 and BRCA2 genes, have been associated with an increased risk of developing prostate cancer.
What is a Digital Rectal Exam (DRE)?
Description of a DRE
A Digital Rectal Exam (DRE) is a physical examination performed by a healthcare professional to assess the prostate gland. During a DRE, the examiner inserts a lubricated, gloved finger into the rectum to feel the back wall of the prostate gland. This allows the examiner to check for any abnormalities, such as enlargement, lumps, or areas of tenderness.
Procedure involved
The procedure for a DRE is relatively simple and usually takes only a few minutes to perform. The healthcare professional will ask you to lie on your side with your knees drawn up to your chest. They will then gently insert their gloved and lubricated finger into the rectum, feeling for any abnormalities in the prostate gland. It is important to communicate any discomfort or pain experienced during the exam to the examiner.
Role of DRE in diagnosing prostate issues
A DRE plays a crucial role in diagnosing prostate issues, including prostate cancer. By physically examining the prostate gland, a healthcare professional can detect any irregularities, such as lumps or enlargement, that may indicate the presence of cancer. However, it is important to note that a DRE alone cannot definitively diagnose prostate cancer and is often used in conjunction with other screening tests.
Traditional Methods of Prostate Cancer Screening
Prostate Specific Antigen (PSA) testing
PSA testing is a blood test that measures the levels of prostate-specific antigen in the blood. PSA is a protein produced by the prostate gland, and high levels may indicate the presence of prostate cancer or other prostate conditions. PSA testing is commonly used as a screening tool for prostate cancer, but it is not without limitations. High PSA levels can also be caused by non-cancerous conditions, such as inflammation or enlargement of the prostate gland.
Transrectal ultrasound (TRUS)
A transrectal ultrasound, or TRUS, uses sound waves to create images of the prostate gland. During the procedure, a small ultrasound probe is inserted into the rectum, which emits sound waves that bounce off the prostate and create detailed images. TRUS can help detect abnormalities in the prostate gland, such as tumors or cysts, and is commonly used alongside other screening methods.
Biopsy and Radiological imaging
A biopsy is the most definitive method of diagnosing prostate cancer. It involves the removal of a small tissue sample from the prostate gland, which is then examined under a microscope for the presence of cancer cells. Radiological imaging techniques, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may also be used to assess the extent of the cancer and evaluate any potential spread to other parts of the body.
The Effectiveness of DRE in Prostate Cancer Screening
Diagnostic accuracy of DRE
While a DRE is a valuable tool in detecting prostate abnormalities, its diagnostic accuracy for prostate cancer is limited. A study published in the Journal of the National Cancer Institute found that the sensitivity of DRE for detecting prostate cancer ranged from 41% to 83%, depending on various factors such as tumor size and location. However, it is important to note that false-negative results are possible, meaning that prostate cancer may go undetected during a DRE.
Comparison of DRE with other screening methods
When compared to other screening methods, such as PSA testing and TRUS, the diagnostic accuracy of DRE is generally lower. PSA testing has been found to be more sensitive in detecting prostate cancer, especially in its early stages. However, combining DRE with PSA testing and other screening methods can increase the overall accuracy of prostate cancer detection.
Variability in DRE findings
The accuracy of a DRE can also vary depending on the skill and experience of the healthcare professional performing the exam. Factors such as the size of the prostate gland, the presence of benign prostatic hyperplasia (BPH), or other prostate conditions can also affect the findings of a DRE. Therefore, it is important to consider other screening methods and consult with a healthcare provider for a comprehensive evaluation.

Occurrence of False-Positives or False-Negatives in DRE
Definition of false-positive and false-negative
A false-positive result occurs when a DRE detects an abnormality in the prostate gland, suggesting the presence of cancer when none is actually present. On the other hand, a false-negative result occurs when a DRE fails to detect prostate cancer, giving a false reassurance that no cancer is present.
Factors that may lead to incorrect DRE results
Several factors can contribute to false-positive or false-negative results in a DRE. These include the examiner's skill and experience, the size and location of the cancerous tumor, the presence of benign conditions that may mimic cancer, and the overall accuracy of the DRE as a screening tool. Additionally, factors such as inflammation, infection, or recent sexual activity can also affect the results of a DRE and may lead to incorrect interpretations.
Consequences of Incorrect DRE Results
Incorrect DRE results can have significant consequences, both emotional and medical. False-positive results can lead to unnecessary anxiety, further invasive testing, and potentially unnecessary treatments. On the other hand, false-negative results can result in delayed or missed diagnosis of prostate cancer, leading to a delay in appropriate treatment and potentially worse outcomes. Therefore, it is essential to consider the limitations and potential inaccuracies of a DRE when interpreting the results.
Benefits of Using DRE for Prostate Cancer Screening
Advantages of DRE
Despite its limitations, a DRE offers certain advantages in prostate cancer screening. It is a relatively simple, cost-effective, and non-invasive procedure that can be performed quickly during a routine medical examination. Additionally, a DRE can help detect other prostate conditions, such as benign prostatic hyperplasia or prostatitis, which may require further evaluation and treatment.
Cases where DRE can be particularly useful
A DRE can be particularly useful in certain cases, such as when a patient has an elevated PSA level or when other screening methods have yielded inconclusive results. It can also help assess the size and consistency of the prostate gland, which can aid in the evaluation of treatment options and disease progression.
Testimonials and positive experiences
Many individuals have reported positive experiences and successful detection of prostate cancer through a DRE. Although anecdotal evidence should not be solely relied upon, these testimonials highlight the potential benefits of a DRE when used in conjunction with other screening methods.

Challenges and Limitations of DRE
Potential discomfort during DRE
For some individuals, a DRE can be an uncomfortable or embarrassing experience. The insertion of a gloved finger into the rectum may cause discomfort or pressure, but it is typically brief and tolerable for most individuals. It is important to communicate any discomfort or concerns with the healthcare professional performing the exam.
Reliance on the examiner's skill and experience
The accuracy and reliability of a DRE are highly dependent on the skill and experience of the healthcare professional performing the exam. Variations in technique, pressure applied, and interpretation of findings may affect the accuracy of the exam. Therefore, it is crucial to choose a healthcare provider who is experienced in performing DREs.
Ambiguous test results
Interpreting the findings of a DRE can sometimes be challenging, as certain factors or conditions may mimic prostate cancer. Enlargement of the prostate due to benign prostatic hyperplasia or inflammation can cause abnormalities that may be mistaken for cancer. In such cases, additional testing, such as PSA testing or a biopsy, may be necessary to confirm the presence or absence of prostate cancer.
Analysis of Studies and Research on DRE's Efficacy
Current research findings
Numerous studies have been conducted to evaluate the efficacy of DRE as a screening tool for prostate cancer. Some studies have reported suboptimal sensitivity and specificity of DRE when used alone. However, other research suggests that combining DRE with other screening tests, such as PSA testing and TRUS, can improve the overall accuracy of prostate cancer detection.
Historical perspective
DRE has been used as a screening tool for prostate cancer for many years, and its role has evolved with the introduction of newer screening methods. It was once considered a routine part of prostate cancer screening, but its standalone efficacy has been questioned in recent years. Nevertheless, it continues to be relevant in certain clinical scenarios and contributes to the comprehensive evaluation of prostate health.
Inferences and conclusions drawn
Based on the available research, it can be inferred that a DRE alone is not sufficient for the definitive diagnosis of prostate cancer. However, when used in conjunction with other screening methods, such as PSA testing and TRUS, it can complement the diagnostic process and aid in the detection of prostate abnormalities. The decision to include DRE as part of a comprehensive screening strategy should be made in consultation with a healthcare provider, taking into consideration individual risk factors and personal preferences.
Alternate Methods for Prostate Cancer Detection
Modern advancements in diagnosis
Advancements in medical technology have led to the development of alternative methods for prostate cancer detection. Magnetic resonance imaging (MRI) and multiparametric MRI (mpMRI) have shown promise in improving the accuracy of prostate cancer detection and localization. Additionally, molecular imaging techniques, such as prostate-specific membrane antigen (PSMA)-PET scans, are emerging as promising tools for detecting and staging prostate cancer.
Pros and cons of alternate methods
These alternate methods offer advantages such as higher sensitivity and specificity compared to traditional methods. They can help identify clinically significant prostate cancer while reducing the detection of insignificant or indolent tumors, which may lead to unnecessary interventions. However, these newer techniques may be more expensive, less readily available, and require specialized expertise for interpretation.
Comparative study of effectiveness
Comparative studies evaluating the effectiveness of alternate methods compared to DRE, PSA testing, and TRUS are ongoing. Preliminary findings suggest that these modern advancements may improve the accuracy of prostate cancer detection and reduce unnecessary biopsies, but further research is needed to establish their role in routine clinical practice.
Making Informed Decisions about Prostate Cancer Screening
Understanding the test results
When undergoing prostate cancer screening, it is essential to understand the test results and their implications. This includes understanding the limitations and potential inaccuracies of each screening method, including DRE. If any abnormalities or concerns are identified, it is important to consult with a healthcare provider to discuss the next steps.
Discussing options and concerns with healthcare provider
Prostate cancer screening should be personalized based on individual risk factors, preferences, and overall health status. It is important to have open and honest discussions with a healthcare provider about the benefits, limitations, and potential risks associated with each screening method, including DRE. This will help ensure that the chosen screening strategy aligns with your specific needs and concerns.
Personalizing your approach to screening
There is no one-size-fits-all approach to prostate cancer screening. Each individual's risk factors and comfort levels may vary, and it is important to personalize the approach to screening accordingly. By considering all available screening methods, discussing concerns with a healthcare provider, and making informed decisions, you can take an active role in the early detection and management of prostate cancer. Remember, proactive screening and open communication are key to maintaining optimal prostate health.