Have you ever wondered what the symptoms of chronic prostatitis are? Understanding a medical condition can often make it less daunting and help you manage it better. Chronic prostatitis, a persistent inflammation of the prostate gland, can manifest in a variety of ways, impacting daily life. Let's take a closer look at the symptoms of chronic prostatitis and how they might affect you.
Understanding Chronic Prostatitis
What is Chronic Prostatitis?
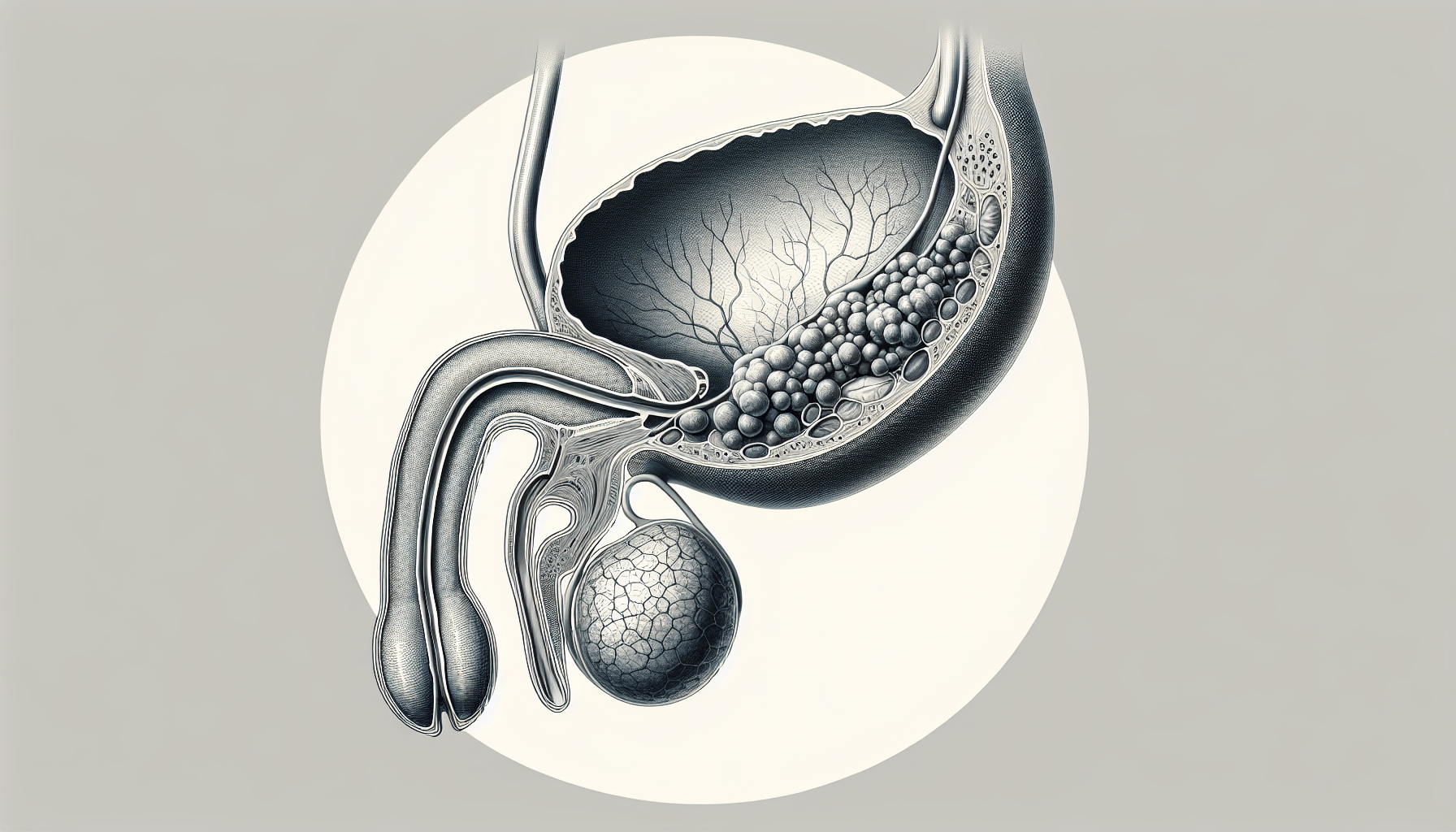
Chronic prostatitis, also known as Chronic Pelvic Pain Syndrome (CPPS), is a condition characterized by prolonged pain and urinary symptoms associated with the prostate gland. Unlike acute prostatitis, which comes on suddenly and can be severe, chronic prostatitis develops more slowly and persists over a longer period.
Types of Chronic Prostatitis
There are different forms of chronic prostatitis, each with its unique characteristics. These include:
| Type | Description |
|---|---|
| Chronic Bacterial Prostatitis | Caused by bacterial infections recurring over a long period. |
| Chronic Non-Bacterial Prostatitis/Chronic Pelvic Pain Syndrome (CPPS) | Characterized by pelvic pain and discomfort without any detectable infection. |
Understanding these types is crucial as symptoms and treatment can vary based on the type of prostatitis.
Common Symptoms of Chronic Prostatitis
The symptoms of chronic prostatitis can be diverse and may vary in intensity. They often overlap with other conditions, making diagnosis sometimes challenging. Here’s a detailed breakdown of the potential symptoms you might experience.
Pain and Discomfort
One of the most prominent signs of chronic prostatitis is persistent pain and discomfort in various parts of the lower body.
Pelvic Pain
Pelvic pain is a hallmark symptom. You might feel a dull ache or sharp pain in the lower abdomen, groin, or perineum (the area between the scrotum and anus).
Genital Pain
Pain can extend to the genitals, including the testicles and penis, which can significantly affect comfort and quality of life.
Lower Back Pain
Chronic prostatitis can also cause pain in the lower back. This discomfort can be mistaken for other common conditions like muscle strain or kidney issues.
Pain During Ejaculation
Experiencing pain during or after ejaculation is another symptom and can affect sexual activity and relationships.
Urinary Symptoms
Urinary symptoms are frequent in chronic prostatitis and can be a significant source of distress.
Frequent Urination
Feel the need to urinate more often than usual? Frequent urination, especially at night (nocturia), is a common complaint.
Urgency
A sudden, strong urge to urinate can occur, often with little warning, which can be inconvenient and embarrassing.
Painful Urination
You may experience a burning or stinging sensation while urinating, medically known as dysuria.
Weak Urine Stream
Difficulty with urinary flow, such as a weak stream or straining to start urination, can indicate obstruction or inflammation.
Sexual Dysfunction
Chronic prostatitis can affect sexual health, leading to various issues.
Erectile Dysfunction
Problems achieving or maintaining an erection can arise, adding to the stress and emotional turmoil caused by the condition.
Decreased Libido
A reduced interest in sexual activity is also commonly reported, often linked with the chronic pain and emotional strain associated with the condition.
Additional Symptoms
Beyond the primary symptoms, other signs might indicate chronic prostatitis. These can sometimes be less specific but still worth noting.
Fatigue
Feeling unusually tired or fatigued, even after adequate rest, can be related to chronic inflammation and pain disrupting your overall well-being.
Emotional Distress
Living with chronic pain and urinary symptoms can take a toll on your mental health, leading to anxiety, depression, and increased stress levels.
Muscle and Joint Pain
Some individuals with chronic prostatitis report experiencing generalized muscle and joint pain, contributing to overall discomfort.
Diagnosing Chronic Prostatitis
The path to diagnosing chronic prostatitis can involve several steps and tests. Here’s a brief overview of what you might expect during the diagnostic process.
Medical History and Physical Examination
Your healthcare provider will begin by taking a detailed medical history and conducting a physical examination, including a digital rectal exam to assess the prostate.
Urine and Prostate Fluid Tests
Laboratory tests on urine and expressed prostate fluid can help identify any infections or abnormalities.
Imaging Tests
In some cases, imaging tests such as ultrasound or MRI may be used to get a clearer view of the prostate and surrounding tissues.
Symptom Scales and Questionnaires
Utilizing specific symptom scales and questionnaires, like the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI), assists in better understanding the severity and impact of your symptoms.
Managing Chronic Prostatitis
While there is no one-size-fits-all treatment for chronic prostatitis, several management strategies can help alleviate symptoms and improve quality of life.
Medications
Various medications can be prescribed, depending on the underlying cause and symptoms.
Antibiotics
If bacterial infection is detected, a course of antibiotics may be necessary. Chronic bacterial prostatitis often requires a longer duration of antibiotic treatment.
Pain Relievers
Over-the-counter pain medications, such as ibuprofen or acetaminophen, can help manage pain and reduce inflammation.
Alpha-Blockers
These medications can help relax the muscles of the bladder neck and prostate, improving urine flow and reducing symptoms.
Physical Therapy
Pelvic floor physical therapy can be beneficial, focusing on relieving muscle tension and reducing pelvic pain.
Lifestyle Changes
Making specific lifestyle changes can also play a significant role in managing symptoms.
Diet and Hydration
Keeping hydrated and avoiding irritants such as caffeine and alcohol can help reduce urinary symptoms.
Stress Management
Incorporating stress management techniques, like mindfulness meditation and yoga, can lessen the emotional and physical impact of chronic prostatitis.
Alternative Therapies
Some individuals find relief with alternative therapies that complement traditional medical treatments.
Acupuncture
Acupuncture may help reduce pain and improve urinary symptoms for some individuals.
Herbal Remedies
Consulting with a healthcare provider about potential herbal remedies could offer additional symptom relief.
When to See a Doctor
Recognizing when to seek professional medical advice is crucial in managing chronic prostatitis effectively.
Persistent Symptoms
If you experience persistent pain, discomfort, or urinary issues that do not improve with standard treatment, it's important to consult a healthcare provider.
Impact on Daily Life
Symptoms that significantly impact your daily activities, work, or relationships warrant a thorough medical evaluation.
New or Worsening Symptoms
Any new or worsening symptoms, such as severe pain, difficulty urinating, or fever, should be promptly addressed to rule out complications or other underlying conditions.
Long-Term Outlook
Living with chronic prostatitis can be challenging, but many individuals find effective ways to manage their symptoms and maintain a good quality of life.
Coping Strategies
Developing personalized coping strategies, such as support groups or counseling, can provide emotional support and practical advice.
Regular Follow-Ups
Regular medical follow-ups and open communication with your healthcare provider can help monitor the condition and adjust treatments as needed.
Healthy Lifestyle
Adopting a healthy lifestyle, including regular exercise, a balanced diet, and stress reduction techniques, plays a significant role in managing chronic prostatitis and overall well-being.
Conclusion
Understanding the symptoms of chronic prostatitis is the first step towards effective management and improving quality of life. By recognizing the diverse ways this condition can manifest, you can work with your healthcare provider to develop a personalized treatment plan. Remember, managing chronic prostatitis is a journey, and with the right strategies and support, you can navigate it more comfortably and confidently.