Prostate cancer, a condition affecting millions of men worldwide, has various treatment options available. From surgery to radiation therapy, hormone therapy to chemotherapy, the choices can be overwhelming. Deciding the best course of action can be a daunting task, but with the support of a healthcare professional and a thorough understanding of the available treatments, you can navigate through the maze of choices and make an informed decision. In this article, we will explore the different treatment options for prostate cancer, shedding light on each approach's benefits and potential side effects, ultimately enabling you to take a step towards your journey of recovery.
Understanding Prostate Cancer
Prostate cancer is a type of cancer that develops in the prostate gland, a small walnut-shaped gland located below the bladder in men. This cancer occurs when the cells in the prostate gland start to grow uncontrollably, forming a tumor. If left untreated, prostate cancer can spread to other parts of the body, such as the bones.
Definition of Prostate Cancer
Prostate cancer is a malignant tumor that forms in the prostate gland. It is one of the most common types of cancer in men, with the majority of cases occurring in older men. The exact cause of prostate cancer is unknown, but certain risk factors, such as age, family history, and ethnicity, can increase the likelihood of developing this disease.
Causes of Prostate Cancer
The exact causes of prostate cancer are not fully understood. However, certain risk factors can increase the chances of developing this disease. Age is a significant risk factor, with prostate cancer more commonly diagnosed in men over the age of 50. Family history plays a role as well, as men with a close relative who has had prostate cancer are at a higher risk. Other factors, such as ethnicity (African-American men have a higher risk) and certain genetic changes, may also contribute to the development of prostate cancer.
Symptoms of Prostate Cancer
In the early stages, prostate cancer may not cause any noticeable symptoms. As the cancer progresses, however, certain signs and symptoms may start to appear. These can include frequent urination, difficulty starting or stopping urination, weak urine flow, blood in the urine or semen, pain or discomfort in the pelvic area, and erectile dysfunction. It is important to remember that having these symptoms does not necessarily mean you have prostate cancer, as they can also be caused by other conditions. If you experience any of these symptoms, it is recommended to see a healthcare professional for further evaluation.
Stages of Prostate Cancer
Prostate cancer is staged based on the extent of the disease and how far it has spread. The most commonly used system for staging prostate cancer is the TNM system, which considers the size of the tumor (T), the involvement of nearby lymph nodes (N), and the presence of distant metastasis (M). The stages range from early-stage (localized) cancer, where the tumor is confined to the prostate gland, to advanced-stage (metastatic) cancer, where the cancer has spread to other parts of the body.
Diagnosing Prostate Cancer
To diagnose prostate cancer, healthcare professionals use a combination of physical examinations, blood tests, imaging tests, and biopsies.
Physical Examination
During a physical examination, your healthcare provider will perform a digital rectal exam (DRE) to feel the size, shape, and texture of your prostate gland. This exam involves the insertion of a gloved, lubricated finger into the rectum to check for any abnormalities.
Blood Tests
A blood test called prostate-specific antigen (PSA) is commonly used to screen for prostate cancer. PSA is a protein produced by the prostate gland, and elevated levels can indicate the presence of prostate cancer. However, a high PSA level does not necessarily mean cancer is present, as it can also be caused by other non-cancerous conditions.
Imaging Tests
Imaging tests, such as ultrasound, magnetic resonance imaging (MRI), or computed tomography (CT) scan, may be ordered to further evaluate the prostate gland and determine the extent of the cancer. These tests can help identify the size and location of the tumor, as well as if the cancer has spread to other areas.
Biopsy
A biopsy is the definitive diagnostic test for prostate cancer. It involves the removal of a small tissue sample from the prostate gland, which is then examined under a microscope for the presence of cancer cells. A biopsy may be performed using a needle guided by ultrasound or MRI imaging. The results of the biopsy will provide information about the grade and stage of the cancer, guiding treatment decisions.
Treatment Decisions
When it comes to treating prostate cancer, several factors need to be considered, including the stage of cancer, overall health, and personal preferences.
Stage of Cancer
The stage of prostate cancer plays a crucial role in determining the most appropriate treatment approach. Treatment options can vary based on whether the cancer is localized, locally advanced, or metastatic. Localized cancer, confined to the prostate gland, may have different treatment options than cancer that has spread to other parts of the body.
Overall Health
A person's overall health and existing medical conditions will also play a role in treatment decisions. Depending on a person's age and overall health status, certain treatments may be more suitable than others. It is essential to consider the potential benefits and risks of each treatment option in relation to the individual's overall health condition.
Personal Preferences
Personal preferences and values are important factors in the treatment decision-making process. The potential side effects and impact on quality of life associated with different treatment options should be discussed with a healthcare provider. This allows individuals to make informed decisions that align with their personal goals, priorities, and values.
Watchful Waiting or Active Surveillance
Definition of Watchful Waiting
Watchful waiting, also known as active surveillance, is a management approach for prostate cancer where immediate treatment is not initiated. Instead, regular monitoring of the cancer is performed to assess its progression.
Advantages of Watchful Waiting
Watchful waiting may be an appropriate choice for individuals with low-risk prostate cancer, where the cancer is slow-growing and less likely to cause significant harm. The advantages of watchful waiting include avoiding the potential side effects of active treatments, such as surgery or radiation therapy, and reserving treatment for cases where the cancer shows signs of progression.
When to consider Watchful Waiting
Watchful waiting is typically recommended for individuals with low-risk prostate cancer or those with limited life expectancy due to age or other health conditions. This approach allows individuals to avoid potential overtreatment and unnecessary side effects, while still maintaining regular monitoring to intervene if the cancer progresses.

Radiation Therapy
Types of Radiation Therapy
Radiation therapy uses high-energy X-rays or other forms of radiation to kill cancer cells or prevent them from growing. There are two primary types of radiation therapy for prostate cancer: external beam radiation therapy (EBRT) and brachytherapy.
Process of Radiation Therapy
During external beam radiation therapy, a machine delivers radiation from outside the body, targeting the prostate gland. The treatment is typically performed in multiple sessions over several weeks. Brachytherapy, on the other hand, involves the insertion of small radioactive seeds directly into the prostate gland. These seeds release radiation over time, effectively targeting the cancer cells.
Side Effects of Radiation Therapy
Radiation therapy can cause side effects, including fatigue, skin changes in the treated area, urinary problems, and bowel changes. These side effects are generally temporary and gradually improve after the completion of treatment. Most individuals experience a good quality of life after radiation therapy, with the side effects becoming less bothersome over time.
Risks Associated with Radiation Therapy
While radiation therapy is an effective treatment option, it does carry some risks. There is a small chance of long-term side effects, such as urinary or bowel problems, erectile dysfunction, and a slightly increased risk of developing a second cancer later in life. It is important to discuss these risks with your healthcare provider to make an informed treatment decision.
Hormone Therapy
Purpose of Hormone Therapy
Hormone therapy, also known as androgen deprivation therapy (ADT), aims to lower the levels of male hormones (androgens) in the body, as these hormones can stimulate the growth of prostate cancer cells. The purpose of hormone therapy is to slow down the growth of the cancer and keep it under control.
Types of Hormone Therapy
There are several types of hormone therapy for prostate cancer. These can include medications that block the production of androgens, medications that block the action of androgens, or surgical removal of the testicles (orchiectomy) to eliminate the source of androgens in the body.
Process of Hormone Therapy
Hormone therapy can be administered through injections, oral medications, or implanted pellets. The duration of treatment can vary, depending on the individual and the stage of the cancer. In some cases, hormone therapy may be used in combination with other treatments, such as radiation therapy or chemotherapy.
Side Effects of Hormone Therapy
Hormone therapy can cause various side effects, including hot flashes, loss of libido, erectile dysfunction, weight gain, fatigue, and mood changes. These side effects can vary in intensity and duration, but can often be managed through lifestyle adjustments, medications, or other interventions. It is important to discuss potential side effects with your healthcare provider before starting hormone therapy.
Risks Associated with Hormone Therapy
While hormone therapy can be effective in controlling prostate cancer, it does carry certain risks. Prolonged use of hormone therapy can lead to bone loss (osteoporosis) and an increased risk of fractures. It is essential to monitor bone health during hormone therapy and consider preventive measures, such as exercise and calcium/vitamin D supplementation.
Surgery (Prostatectomy)
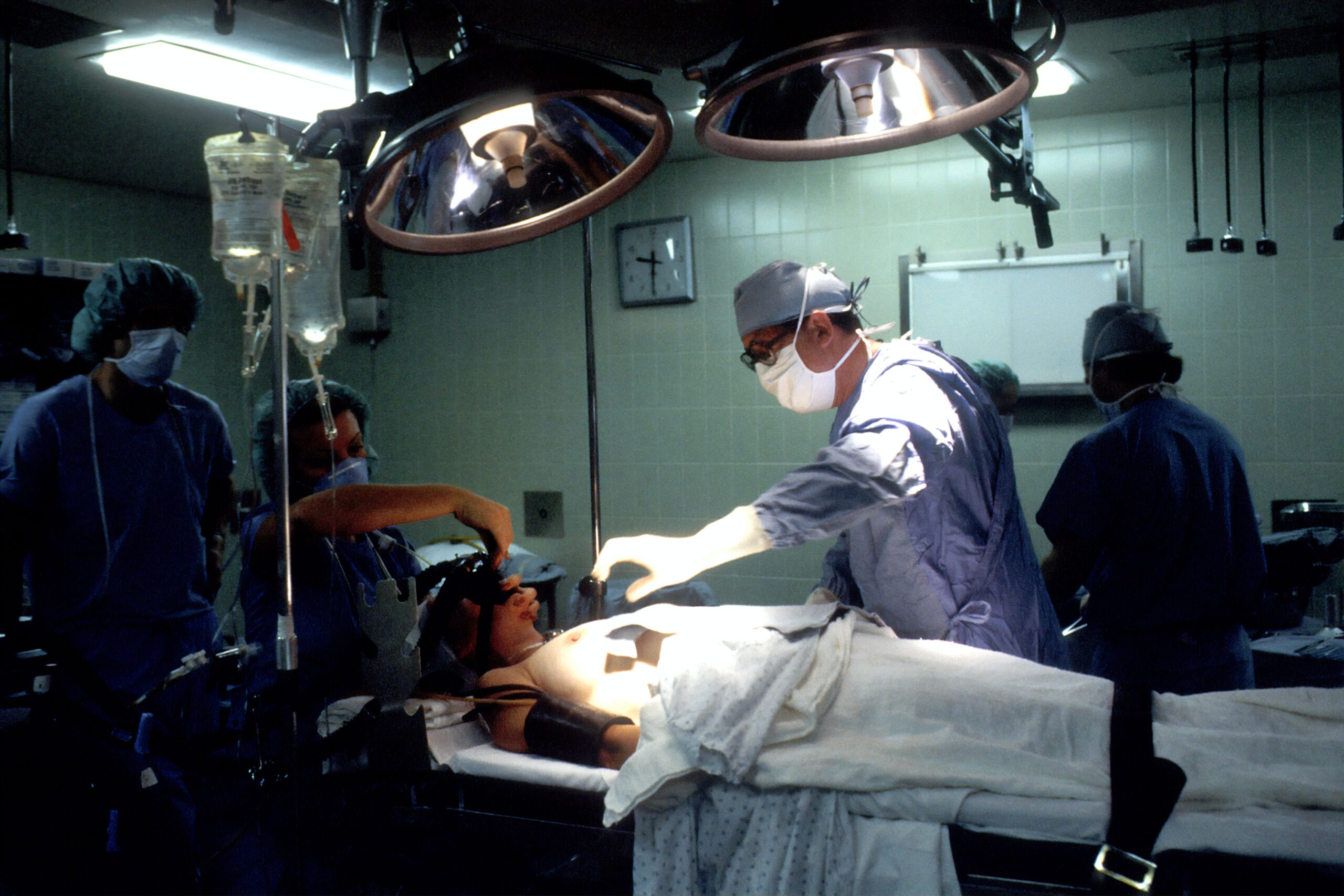
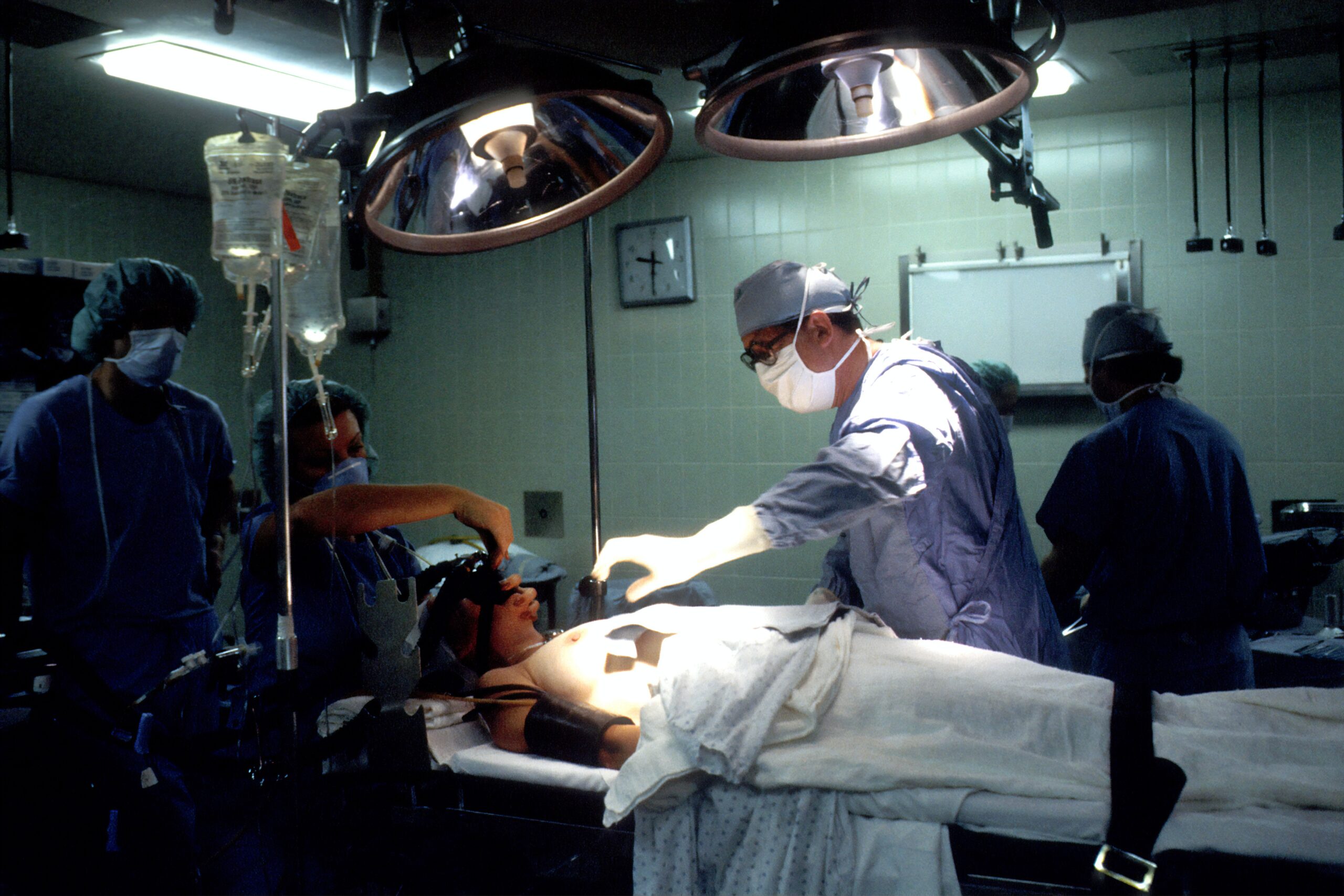
Procedure of Prostatectomy
Prostatectomy is a surgical procedure that involves the removal of the prostate gland and surrounding tissues. There are different approaches to prostatectomy, including open surgery, laparoscopic surgery, and robotic-assisted surgery. The choice of approach depends on various factors, including the surgeon's expertise and the individual's specific circumstances.
Preparation for Prostatectomy
Prior to undergoing prostatectomy, individuals may need to undergo certain preparatory steps, such as medical evaluations, blood tests, and discontinuing certain medications. It is essential to follow the preoperative instructions provided by the healthcare team to ensure a successful surgery and optimal recovery.
Recovery from Prostatectomy
After prostatectomy, individuals may experience a recovery period that involves physical healing and adjustment to changes in urinary and sexual function. It is normal to experience some discomfort and urinary leakage in the immediate postoperative period. With appropriate care and rehabilitation, most individuals regain urinary control and resume sexual activity within a few months of surgery.
Risks and Complications of Prostatectomy
Like any surgical procedure, prostatectomy carries a risk of complications. These can include bleeding, infection, blood clots, urinary incontinence, erectile dysfunction, and damage to surrounding structures. The risk of complications varies depending on factors such as the individual's overall health, surgical technique, and surgeon's experience. It is important to discuss the potential risks with your surgeon before proceeding with prostatectomy.
High Intensity Focused Ultrasound (HIFU)
Understanding HIFU
High Intensity Focused Ultrasound (HIFU) is a non-invasive treatment option for prostate cancer. It uses ultrasound waves to create heat, which destroys cancer cells in the prostate gland.
Procedure of HIFU
During HIFU treatment, an ultrasound probe is placed in the rectum, allowing precise targeting of the prostate gland. The ultrasound waves generate heat, effectively ablating the cancer cells within the prostate. HIFU is typically performed as an outpatient procedure, and patients generally recover quickly with minimal side effects.
Benefits of HIFU
HIFU offers several benefits for the treatment of prostate cancer. It is a non-invasive procedure that does not require surgical incisions, resulting in minimal blood loss and a shorter recovery time compared to traditional surgical treatments. HIFU also offers precise targeting of the cancer cells, reducing the risk of damage to surrounding healthy tissues.
Risks Associated with HIFU
While HIFU is generally considered safe, it does carry some risks. Potential side effects can include urinary problems (such as urinary incontinence or difficulty urinating), erectile dysfunction, and rectal complications. It is important to discuss the potential risks and benefits of HIFU with your healthcare provider to make an informed treatment decision.
Chemotherapy
How Chemotherapy Works
Chemotherapy is a systemic treatment for prostate cancer that uses drugs to kill cancer cells or slow down their growth. Unlike other treatment options, chemotherapy affects the entire body, targeting cancer cells wherever they may be.
Process of Chemotherapy
Chemotherapy for prostate cancer is typically administered intravenously, meaning the drugs are delivered through a vein. The treatment is usually given in cycles, with rest periods in between to allow the body to recover. The specific drugs and treatment plan may vary depending on the individual's condition and the stage of the cancer.
Side Effects of Chemotherapy
Chemotherapy can cause various side effects, as the drugs target rapidly dividing cells, including both cancer cells and healthy cells. Common side effects can include fatigue, hair loss, nausea, vomiting, diarrhea, and increased risk of infection. These side effects are usually temporary and can be managed with supportive care measures and medications.
Who should consider Chemotherapy
Chemotherapy is typically reserved for prostate cancer cases that have advanced to a metastatic stage or have not responded to other treatments. It may also be used in combination with other treatment modalities to enhance the effectiveness of treatment. The decision to undergo chemotherapy should be made in consultation with a healthcare provider, considering the individual's specific situation and overall health.
Living with Prostate Cancer
Maintaining a Healthy Lifestyle
Living with prostate cancer involves adopting a healthy lifestyle that can help manage the disease and improve overall well-being. This includes eating a balanced diet, engaging in regular physical activity, maintaining a healthy weight, avoiding tobacco and excessive alcohol consumption, and managing stress levels.
Managing Side Effects
Many treatments for prostate cancer can cause side effects that impact daily life. It is essential to communicate openly with healthcare providers about any side effects experienced. There are often strategies and medications available to help manage side effects, such as urinary incontinence, erectile dysfunction, or fatigue.
Psychological and Emotional Support
Prostate cancer diagnosis and treatment can have a significant impact on a person's emotional well-being. It is important to seek appropriate psychological support, whether through counseling, support groups, or talking with friends and family. Emotional support can help individuals cope with the challenges of prostate cancer and maintain a positive outlook.
Regular Follow-ups
Regular follow-up appointments with healthcare providers are crucial to monitor the progress of prostate cancer, manage any side effects, and address any concerns or questions that may arise. These appointments often include physical examinations, blood tests, imaging tests, and discussions about treatment options. Following the recommended follow-up schedule can help ensure optimal management and early detection of any changes or progression of the cancer.
In conclusion, understanding prostate cancer and the available treatment options is crucial for making informed decisions about managing this condition. Each treatment modality has its own advantages, risks, and considerations. By working closely with healthcare professionals and considering personal preferences and overall health, individuals can embark on a treatment plan that is tailored to their specific needs, ensuring the best possible outcomes in their journey with prostate cancer.