Have you ever wondered if an infection in the prostate gland could potentially lead to cancer? In this article, we will explore the link between prostate gland infections and the development of cancer. Exploring the possibility of such a connection can help us better understand the risks and take necessary precautions to maintain our prostate health. So, let's uncover the truth behind this intriguing question together. Understanding The Prostate Gland
Overview of the prostate gland
The prostate gland is a small, walnut-sized gland located just below the bladder in men. It is an important part of the male reproductive system, producing and secreting fluid that helps nourish and transport sperm. The prostate gland surrounds the urethra, the tube that carries urine and semen out of the body.
Function of the prostate gland
The primary function of the prostate gland is to produce and secrete the fluid that makes up a significant portion of semen. This fluid helps dilute and protect sperm, increasing their chances of successfully fertilizing an egg. Additionally, the prostate gland has a muscular component that aids in the expulsion of semen during ejaculation.
Location and size of the prostate gland
The prostate gland is located just below the bladder, in front of the rectum. Its position allows it to be palpated during a physical examination. The size of the prostate gland varies among individuals and tends to grow larger as men age. In younger men, it is typically about the size of a walnut, while in older men, it can increase to the size of a small plum or even larger.
Prostate Infections
Types of prostate infections
There are two main types of prostate infections: acute bacterial prostatitis and chronic bacterial prostatitis. Acute bacterial prostatitis is a sudden and severe infection caused by bacteria entering the prostate gland. It typically presents with symptoms such as fever, chills, pain in the lower back or pelvic area, frequent urination, and difficulty urinating. Chronic bacterial prostatitis, on the other hand, is a recurring infection that lasts for an extended period. Symptoms may be less severe but can last for several months or even years.
Causes of prostate infections
Prostate infections are commonly caused by bacteria, usually from the urinary tract or rectum. The bacteria can enter the prostate via the urethra or bloodstream. In some cases, a urinary tract infection or an untreated bladder infection can lead to a prostate infection. Other risk factors include urinary catheterization, a recent prostate biopsy, or a weakened immune system.
Symptoms of prostate infections
The symptoms of prostate infections can vary depending on the type and severity of the infection. Common symptoms include pain or discomfort in the pelvic area, frequent urination, pain or burning during urination, difficulty urinating, blood in the urine, and flu-like symptoms such as fever, chills, and body aches.
Treatment of prostate infections
Prostate infections are typically treated with antibiotics to target and eliminate the bacterial infection. The specific antibiotic prescribed will depend on the type of bacteria causing the infection. In severe cases or cases where there are complications, hospitalization may be necessary. Besides antibiotics, pain relievers may be prescribed to manage discomfort, and warm baths or sitz baths can provide temporary relief. It is important to complete the full course of antibiotics prescribed, even if symptoms improve, to ensure complete eradication of the infection.
Prevalence of Prostate Cancer
Prostate cancer statistics worldwide
Prostate cancer is one of the most common cancers among men worldwide. According to the World Health Organization (WHO), prostate cancer is responsible for approximately 1.3 million new cases and over 350,000 deaths annually. The incidence of prostate cancer varies geographically, with higher rates in North America, Europe, and Australia. It is important to note that these statistics are general estimates, and individual risk factors can influence an individual's likelihood of developing prostate cancer.
Risk factors for prostate cancer
Several risk factors increase the chances of developing prostate cancer. Age is a significant risk factor, with the incidence of prostate cancer increasing with age. Family history and genetics also play a role, as men with a close relative, such as a father or brother, who has had prostate cancer are at higher risk. Ethnicity can also impact the risk, with African-American men having a higher incidence and mortality rate compared to other racial and ethnic groups. Other risk factors include obesity, a high-fat diet, and exposure to certain chemicals or toxins.
Symptoms of prostate cancer
In the early stages, prostate cancer may not cause any noticeable symptoms. As the cancer progresses, however, symptoms may emerge. These can include urinary problems such as frequent urination, weak urine flow, difficulty starting or stopping urination, blood in the urine or semen, erectile dysfunction, pain or discomfort in the pelvic area, and bone pain. It is important to note that these symptoms can also be caused by other conditions, so it is essential to consult a healthcare professional for proper diagnosis.
Understanding The Prostate Cancer
Pathophysiology of prostate cancer
Prostate cancer develops when the cells in the prostate gland grow and divide abnormally, forming a tumor. The exact cause of these abnormal cell growth is not fully understood, but it is believed to be a result of genetic mutations. These mutations alter the normal control mechanisms of cell growth and division, causing the cells to multiply uncontrollably and form a malignant tumor.
Different stages of prostate cancer
Prostate cancer is typically classified into different stages based on the extent of the disease and how far it has spread. The staging system commonly used is the TNM system, which stands for Tumor, Node, and Metastasis. The T stage refers to the size and extent of the primary tumor, the N stage indicates the involvement of nearby lymph nodes, and the M stage describes the presence of metastasis or spread to distant sites.
Prostate cancer prognosis
The prognosis for prostate cancer varies depending on several factors, including the stage of the cancer at diagnosis, the individual's overall health, and the aggressiveness of the tumor. Prostate cancer is often slow-growing and may not require immediate treatment. However, in some cases, the cancer can be aggressive and spread quickly. Early detection and treatment significantly improve the prognosis and increase the chances of successful treatment.
Link Between Prostate Infections and Cancer
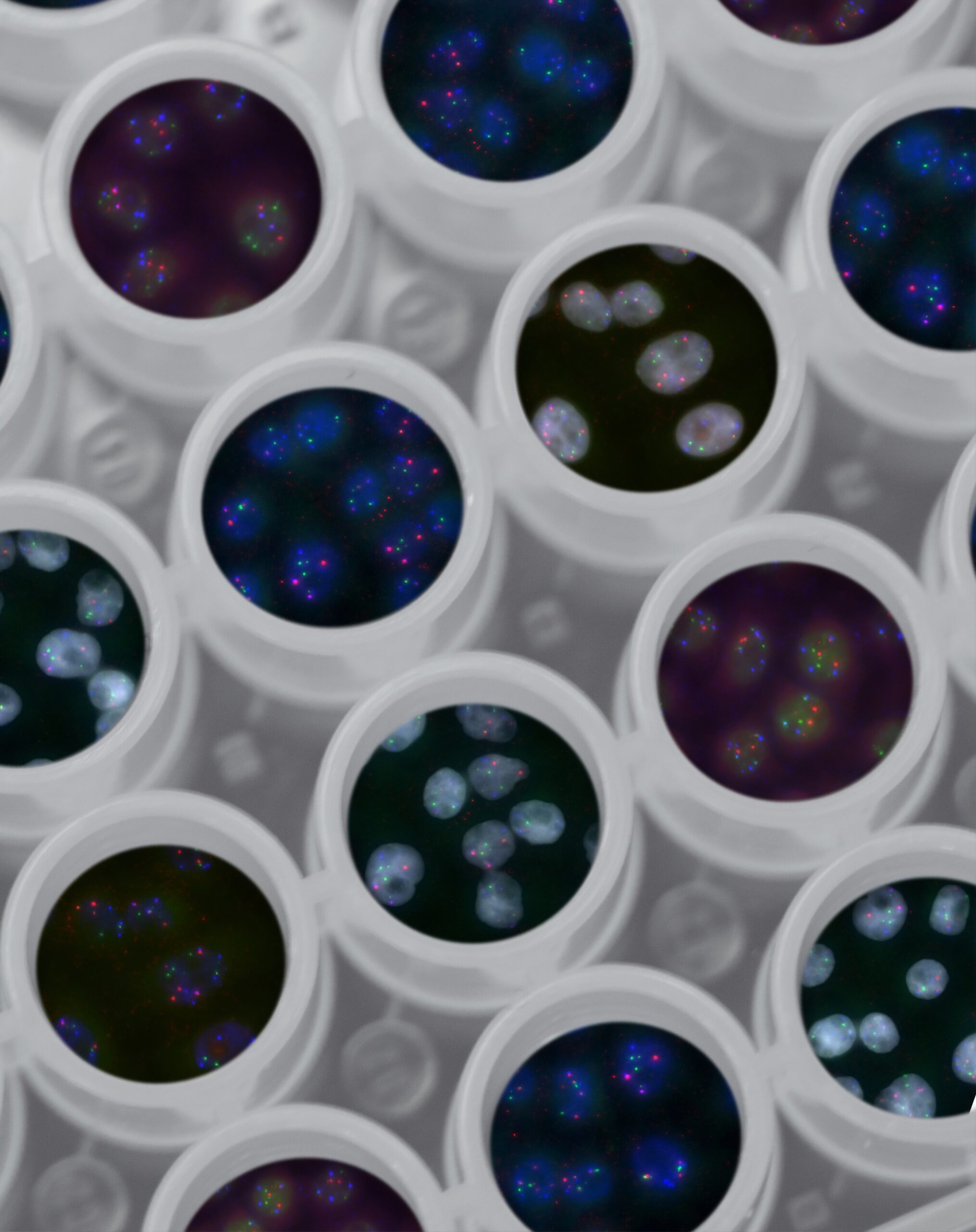
Existing research on the connection
The link between prostate infections and cancer is a subject of ongoing research. Several studies have explored this connection, but the evidence remains inconclusive. Some research suggests that chronic inflammation caused by recurrent prostate infections may contribute to the development of prostate cancer. However, more studies are needed to establish a definitive link and understand the underlying mechanisms.

Inflammation as a potential trigger for cancer
Inflammation is a natural immune response that occurs when the body is fighting an infection or injury. It is characterized by redness, swelling, and pain. Chronic or long-term inflammation can potentially damage cells and DNA, leading to genetic mutations that can increase the risk of cancer development. In the case of prostate infections, the persistent inflammation may create an environment prone to the initiation and progression of cancerous cells.
Critiques and controversies around the link
The link between prostate infections and cancer is a topic of debate in the scientific community. Critics argue that the evidence connecting the two is not strong enough to establish a causal relationship. They suggest that other factors, such as genetic predisposition or shared risk factors, may be responsible for both prostate infections and the development of cancer. Additionally, some sources of bias or confounding variables in studies examining the link may influence the results, yielding conflicting findings.
The Role of Sexually Transmitted Infections
Overview of STIs and prostate health
Sexually transmitted infections (STIs) are infections that are primarily transmitted through sexual contact. While STIs primarily affect the sexual and reproductive organs, they can also have an impact on prostate health. Certain STIs, such as gonorrhea and chlamydia, can cause inflammation and infection in the prostate gland. This inflammation may contribute to long-term prostate health issues, potentially increasing the risk of developing prostate cancer.
Studies linking STIs to prostate cancer
Several studies have investigated the link between certain STIs and prostate cancer. Research suggests that certain sexually transmitted bacteria, such as those causing gonorrhea and chlamydia, may be associated with an increased risk of developing prostate cancer. These bacteria can infect the prostate gland and cause chronic inflammation, potentially leading to the development of cancerous cells over time. However, further research is needed to fully understand and confirm this link.
Potential reasons for this correlation
The correlation between STIs and prostate cancer may be attributed to the chronic inflammation caused by these infections. Inflammation in the prostate gland can trigger a series of cellular responses that can lead to genetic mutations and the development of cancer cells. Additionally, some STIs may directly damage the DNA of prostate cells, further increasing the risk of cancer development. However, it is important to note that not all individuals with a history of STIs will develop prostate cancer, and other factors may contribute to the overall risk.
Impact of Lifestyle and Prevention
Influence of diet and exercise on prostate health
Maintaining a healthy lifestyle can play a significant role in prostate health and potentially reduce the risk of prostate-related issues, including prostate cancer. Regular physical activity, such as brisk walking or moderate-intensity exercise, has been associated with a lower risk of developing prostate cancer. A well-balanced diet that includes a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats can also contribute to prostate health. Limiting the consumption of red and processed meats, as well as high-fat foods, is recommended.
Sexual activity and prostate health
Research suggests that sexual activity may have some impact on prostate health. Some studies have found that frequent ejaculation, either through sexual activity or masturbation, may be associated with a lower risk of developing prostate cancer. Although the exact reason for this association is not fully understood, it is believed that regular ejaculation helps flush out potentially harmful substances from the prostate.

Antioxidants and anti-inflammatory foods
Certain foods rich in antioxidants and anti-inflammatory properties may have a positive impact on prostate health. Foods such as tomatoes, berries, green tea, cruciferous vegetables (broccoli, cauliflower, Brussels sprouts), and fatty fish (salmon, sardines) contain beneficial compounds that can reduce inflammation and protect against cellular damage. Including these foods in a balanced diet can contribute to overall prostate health.
Role of Medical Screening
Importance of regular prostate exams
Regular prostate exams are crucial for ensuring early detection of any potential issues, including prostate cancer. Prostate exams typically involve a physical examination of the prostate gland, known as a digital rectal examination (DRE), as well as a blood test called prostate-specific antigen (PSA) test. These exams can help detect any abnormalities or signs of prostate problems, including enlarged prostate or cancer, even before noticeable symptoms appear.
PSA test for early detection of prostate cancer
The PSA test measures the level of prostate-specific antigen in the blood, which can be elevated in the presence of prostate cancer. It serves as a screening tool to detect potential prostate cancer early. However, it is important to note that an elevated PSA level does not necessarily indicate cancer, as other factors can also elevate PSA levels. Further diagnostic tests, such as a biopsy, may be necessary to confirm or rule out prostate cancer.
Debates around screening practices
There are ongoing debates and controversies surrounding prostate cancer screening practices, particularly regarding the PSA test. Critics argue that the PSA test can lead to false positives and unnecessary invasive procedures, such as biopsies, resulting in potential harm and anxiety for the patients. Others emphasize the importance of early detection and believe that regular screening can help detect prostate cancer at an early, more treatable stage. It is important for individuals to discuss the potential benefits and risks of screening with their healthcare provider to make an informed decision.
Treatment Options for Prostate Cancer
Surgical procedures
Surgical procedures are commonly employed in the treatment of prostate cancer, depending on the stage and extent of the disease. The main surgical option is a radical prostatectomy, which involves the removal of the entire prostate gland. This procedure can be done through open surgery or minimally invasive techniques, such as laparoscopic or robot-assisted surgery. Other surgical options, such as transurethral resection of the prostate (TURP), may be used to treat localized or less aggressive cases of prostate cancer.
Radiation therapy
Radiation therapy uses high-energy rays to kill cancer cells and shrink tumors. It can be administered externally through external beam radiation therapy, which targets the prostate gland from outside the body, or internally through brachytherapy, where radioactive seeds are inserted directly into the prostate. Radiation therapy is often used as the primary treatment for localized prostate cancer or in combination with other treatment modalities.
Hormone therapy
Hormone therapy, also known as androgen deprivation therapy (ADT), aims to reduce the levels of male hormones, particularly testosterone, in the body. Prostate cancer cells rely on these hormones for growth, and by reducing their levels, hormone therapy can help slow down or prevent the growth of cancer cells. Hormone therapy can be administered through medications that block the production or action of testosterone or through surgical removal of the testicles (orchidectomy).
Watchful waiting
Watchful waiting, also known as active surveillance, is an approach often employed for slow-growing or low-risk prostate cancer. Instead of initiating immediate treatment, the patient and healthcare team closely monitor the cancer's progression through regular check-ups, prostate-specific antigen (PSA) tests, and other imaging studies. If there are signs of progression or worsening, treatment options can be reconsidered.
New advances in treatment
Advances in medical research and technology continue to expand the treatment options for prostate cancer. Emerging therapies, such as immunotherapy, targeted therapies, and focal therapy, are being investigated and may offer more precise and individualized treatment approaches. Clinical trials are ongoing to evaluate the efficacy and safety of these new treatment modalities, providing hope for improved outcomes and quality of life for individuals diagnosed with prostate cancer.
Significance of Early Diagnosis
Impact of early detection on survival rates
Early detection of prostate cancer significantly improves the chances of successful treatment and long-term survival. When prostate cancer is diagnosed at an early stage and confined to the prostate gland, the five-year survival rate approaches nearly 100%. However, if the cancer has already spread to distant organs or lymph nodes, the five-year survival rate drops dramatically. Regular screenings and prompt medical attention can help identify prostate cancer at an early, potentially curable stage.
Quality of life post-diagnosis
The impact of prostate cancer on an individual's quality of life can vary depending on various factors, such as the stage of the disease, the treatment received, and the individual's overall health. Treatment options, such as surgery or radiation therapy, can cause side effects, including urinary incontinence, erectile dysfunction, and bowel problems. However, advancements in treatment techniques have led to improved outcomes and reduced side effects, allowing many individuals to maintain a good quality of life even after a prostate cancer diagnosis.
Strategies for improving early diagnosis rates
To improve early diagnosis rates, it is crucial to raise awareness about the importance of regular screening and early detection of prostate cancer. Education campaigns can help inform individuals about the risk factors, symptoms, and available screening options. Encouraging open conversations between healthcare providers and patients can also facilitate discussions about the potential benefits and risks of screening and ensure informed decision-making. Additionally, ongoing research on new diagnostic tools and biomarkers can further enhance the accuracy and effectiveness of early detection methods.

