Let's talk about common prostate disorders that you might encounter at some point. Your prostate, a small gland located below the bladder, plays a vital role in the male reproductive system. While it often remains unnoticed, issues related to the prostate can cause discomfort and affect your overall health. From enlarged prostate to prostatitis, this article will shed light on these conditions, their symptoms, and available treatments. So, let's dive into the world of prostate disorders and learn more about these common ailments that you should be aware of.
Prostate Cancer
Understanding Prostate Cancer
Prostate cancer is a type of cancer that occurs in the prostate gland, which is a small walnut-shaped organ located just below the bladder in men. It is one of the most common types of cancer among men, but with early detection and proper treatment, it has a high survival rate. Prostate cancer develops when the cells in the prostate gland begin to grow out of control, forming a tumor. These cancerous cells can spread to other parts of the body if not detected and treated in the early stages.
Risk Factors for Prostate Cancer
While the exact cause of prostate cancer is unknown, there are several factors that can increase your risk of developing this disease. Age is one of the most significant risk factors, as the risk of prostate cancer increases with age. Other risk factors include family history, with men who have a close relative with prostate cancer being at a higher risk, as well as race, with African American men having a higher incidence rate compared to other racial/ethnic groups. Other factors such as obesity, smoking, and certain genetic mutations may also play a role in increasing the risk of prostate cancer.
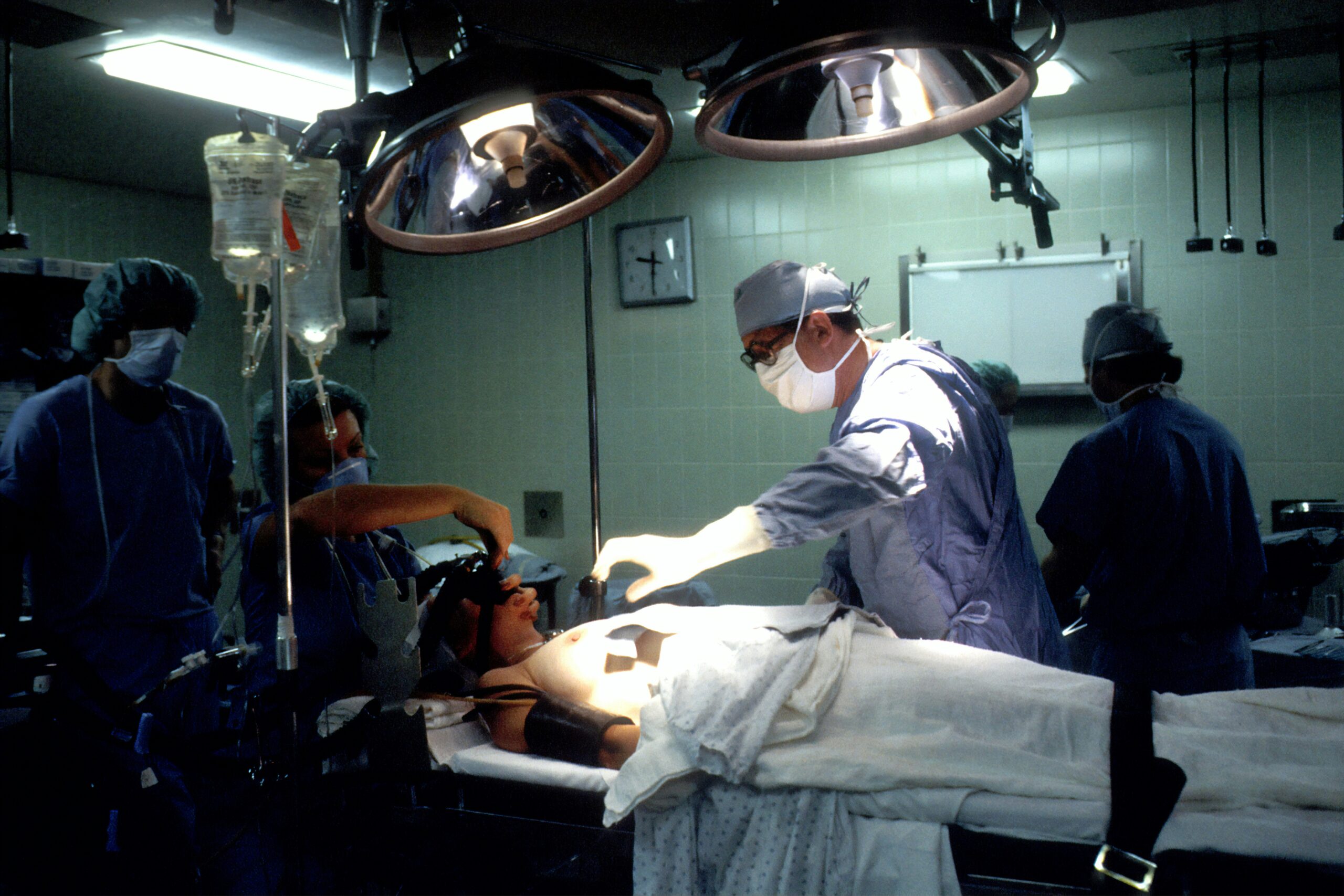
Diagnosis and Treatment of Prostate Cancer
Early detection of prostate cancer is crucial for effective treatment and improved outcomes. There are several methods used for diagnosing prostate cancer, including a prostate-specific antigen (PSA) blood test, a digital rectal exam (DRE), and imaging tests such as a transrectal ultrasound (TRUS) or a biopsy of the prostate. Treatment options for prostate cancer depend on various factors, including the stage of the cancer, the aggressiveness of the tumor, and the overall health of the individual. Treatment options may include surgery, radiation therapy, chemotherapy, hormone therapy, or a combination of these approaches. The choice of treatment is best made in consultation with a healthcare professional who can provide personalized recommendations.
Benign Prostatic Hyperplasia (BPH)
Understanding Benign Prostatic Hyperplasia
Benign Prostatic Hyperplasia (BPH) is a non-cancerous condition that affects the prostate gland. It occurs when the prostate gland enlarges and puts pressure on the urethra, the tube that carries urine from the bladder out of the body. BPH is a common condition that typically affects older men and can cause bothersome urinary symptoms. While BPH is not considered a life-threatening condition, it can significantly impact a man's quality of life if left untreated.
Signs and Symptoms of BPH
The signs and symptoms of BPH can vary from person to person but commonly include urinary frequency, urgency, weak urine flow, difficulty starting or stopping urination, and the need to wake up frequently at night to urinate. These symptoms can be bothersome and may affect your daily activities and sleep quality. If you are experiencing any of these symptoms, it is essential to consult a healthcare professional for an accurate diagnosis and appropriate management.
Treatment Options for BPH
The treatment options for BPH depend on the severity of symptoms and the impact on your quality of life. In mild cases, lifestyle changes such as limiting fluid intake before bedtime, avoiding caffeine and alcohol, and practicing bladder training exercises may help alleviate symptoms. Medications can also be prescribed to relieve symptoms and shrink the prostate gland. In more severe cases, surgical intervention may be necessary. Procedures such as transurethral resection of the prostate (TURP), laser therapy, and other minimally invasive techniques can effectively reduce prostate size and improve urinary symptoms.

Prostatitis
Understanding Prostatitis
Prostatitis refers to the inflammation of the prostate gland and can be caused by various factors, including infection, urinary tract abnormalities, or autoimmune disorders. It is classified into four different types: acute bacterial prostatitis, chronic bacterial prostatitis, chronic pelvic pain syndrome, and asymptomatic inflammatory prostatitis. Prostatitis can cause discomfort and pain in the pelvic area, as well as urinary symptoms similar to those seen in other prostate disorders.
Types of Prostatitis
-
Acute bacterial prostatitis: This type of prostatitis is caused by a bacterial infection and typically comes on suddenly with severe symptoms such as fever, chills, pain in the lower abdomen or back, frequent urination, and pain during urination.
-
Chronic bacterial prostatitis: This type of prostatitis occurs when bacteria persistently infect the prostate gland. Symptoms may be less severe but can last for an extended period, with recurrent urinary tract infections and pelvic pain.
-
Chronic pelvic pain syndrome: This is the most common form of prostatitis and is characterized by long-term pelvic pain and urinary symptoms. The exact cause is unknown, but it may involve inflammation, muscle dysfunction, or nerve damage.
-
Asymptomatic inflammatory prostatitis: This type of prostatitis does not cause symptoms and is usually diagnosed incidentally during testing for other conditions.
Diagnosis and Treatment of Prostatitis
The diagnosis of prostatitis involves a physical examination, medical history review, and various tests, such as a urine sample analysis, prostate fluid analysis, or imaging studies. Treatment options for prostatitis depend on the underlying cause and type of prostatitis diagnosed. Antibiotics are usually prescribed for acute bacterial prostatitis and chronic bacterial prostatitis. For chronic pelvic pain syndrome, treatment may involve a combination of medications to manage symptoms, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or alpha-blockers, as well as physical therapy or relaxation techniques. Asymptomatic inflammatory prostatitis may not require treatment unless symptoms develop.
Prostate Stones
Understanding Prostate Stones
Prostate stones, also known as prostatic calculi, are small mineral deposits that can form in the prostate gland. These stones are generally harmless and can vary in size from small sand-like grains to larger stones that can obstruct the urinary tract. While the exact cause of prostate stones is unknown, they are believed to develop when certain substances crystallize within the prostate gland.
Causes and Symptoms of Prostate Stones
The exact causes of prostate stones are not well understood, but they may be associated with chronic prostatitis, prostate enlargement (BPH), or ductal blockage within the prostate gland. Prostate stones are more common in older men and can be asymptomatic in many cases. However, they can cause urinary symptoms such as frequent urination, weak urine flow, or difficulty emptying the bladder fully. In some cases, larger stones may lead to urinary tract infections or bladder obstruction, requiring medical intervention.
Treatment of Prostate Stones
In many cases, prostate stones do not require treatment if they are not causing significant symptoms or complications. However, if the stones are causing bothersome urinary symptoms or recurrent infections, treatment options may include medication to help relax the prostate muscles or alpha-blockers to improve urine flow. In cases where the stones are large and causing blockage or severe symptoms, surgical intervention may be necessary to remove the stones. Procedures such as transurethral prostatectomy or lithotripsy can help break up or remove the stones, allowing for improved urinary function.

Prostate Abscess
Understanding Prostate Abscess
A prostate abscess is a rare but serious condition characterized by the formation of a pus-filled cavity within the prostate gland. It usually occurs as a complication of acute bacterial prostatitis or as a result of a spreading infection from nearby organs. A prostate abscess can cause severe pain, fever, and urinary symptoms, and requires immediate medical attention.
Causes and Symptoms of Prostate Abscess
The most common cause of a prostate abscess is an infection that spreads to the prostate gland, usually from the urinary tract or the bloodstream. Bacterial prostatitis, particularly the acute bacterial type, is the most common predisposing factor. The symptoms of a prostate abscess may include severe pain in the lower abdomen or back, fever, chills, difficulty urinating, frequent urination, and a general feeling of illness. Prompt diagnosis and treatment are crucial to prevent complications such as the spread of infection to other parts of the body.
Treatment of Prostate Abscess
The treatment of a prostate abscess usually involves a combination of medical and surgical interventions. Antibiotics are typically prescribed to control the infection, and drainage of the abscess may be necessary. In some cases, a tube may be inserted through the skin into the abscess to facilitate drainage. Surgical drainage may be required if the abscess does not respond to conservative treatment or if there is a risk of complications. The specific approach to treatment will depend on the severity of the abscess and the individual's overall health.
Prostatic Cysts
Understanding Prostatic Cysts
Prostatic cysts are fluid-filled sacs that can develop within the prostate gland. These cysts are usually benign and can vary in size from tiny cysts that go unnoticed to larger cysts that can cause urinary symptoms or other complications. The exact cause of prostatic cysts is unknown, but they are thought to develop from ductal blockages or inflammation within the prostate gland.
Risk Factors and Symptoms of Prostatic Cysts
Prostatic cysts are more common in older men and may be associated with other prostate disorders such as BPH or chronic prostatitis. In many cases, prostatic cysts are asymptomatic and do not require treatment. However, larger cysts can cause urinary symptoms such as frequent urination, weak urine flow, or difficulty emptying the bladder completely. In some cases, prostatic cysts may become infected, leading to more severe symptoms such as fever, chills, or pain in the pelvic area.
Diagnosis and Treatment of Prostatic Cysts
The diagnosis of prostatic cysts typically involves a physical examination, medical history review, and imaging studies such as transrectal ultrasound (TRUS) or magnetic resonance imaging (MRI). Treatment for prostatic cysts depends on the size and symptoms. Small, asymptomatic cysts may not require treatment but may be monitored periodically. If the cysts are causing symptoms or complications, drainage or surgical removal of the cyst may be necessary. This can be done through minimally invasive procedures such as transurethral resection or needle aspiration.
Prostate Atrophy
Understanding Prostate Atrophy
Prostate atrophy refers to the shrinkage or reduction in size of the prostate gland. It is a common age-related change that can occur in men as they get older. Prostate atrophy does not usually cause symptoms or health problems, but it may be associated with other prostate disorders such as BPH or prostatitis.
Causes and Symptoms of Prostate Atrophy
The exact causes of prostate atrophy are not well understood, but hormonal changes, inflammation, and aging are believed to play a role. Prostate atrophy is more common in older men and may be associated with a decrease in testosterone levels. While prostate atrophy itself does not typically cause symptoms, it may be associated with urinary symptoms seen in other prostate disorders, such as BPH.
Treatment of Prostate Atrophy
Prostate atrophy generally does not require treatment unless it is causing bothersome urinary symptoms or is associated with other prostate disorders. In such cases, the treatment will depend on the specific condition or symptoms present. For example, if BPH is causing urinary symptoms, treatment options may include medications to relax the prostate muscles or surgery to remove or reduce the size of the prostate gland. It is important to consult with a healthcare professional for a proper diagnosis and personalized treatment plan.
Prostate Infarction
Understanding Prostate Infarction
Prostate infarction refers to the death of prostate tissue due to inadequate blood supply, typically caused by a blockage or clot in the blood vessels that supply the prostate gland. It is a rare condition that can cause severe pain and lead to complications such as abscess formation or urinary problems.
Symptoms and Causes of Prostate Infarction
The exact cause of prostate infarction is not always clear, but it is believed to result from a disruption in the blood flow to the prostate gland. This can occur due to various factors, including blood clots, inflammation of the blood vessels, or trauma. The symptoms of prostate infarction may include severe pain in the lower abdomen or pelvic area, difficulty urinating, blood in the urine, or symptoms similar to acute bacterial prostatitis. Prompt medical attention is necessary to prevent complications and alleviate symptoms.
Treatment of Prostate Infarction
The treatment of prostate infarction typically involves a combination of medical and surgical interventions. Antibiotics may be prescribed to control any infection present, and pain management medications may be given to alleviate discomfort. In some cases, drainage of abscesses or surgical removal of affected tissue may be necessary. Treatment decisions will depend on the severity of the condition and the individual's overall health.
Chronic Pelvic Pain Syndrome (CPPS)
Understanding Chronic Pelvic Pain Syndrome
Chronic Pelvic Pain Syndrome (CPPS), also known as chronic prostatitis, is a common condition characterized by long-term pelvic pain and discomfort. It is one of the most challenging prostate disorders to diagnose and treat, as its exact cause is often unknown. CPPS can significantly impact a man's quality of life, causing physical and emotional distress.
Symptoms and Causes of CPPS
The symptoms of CPPS can vary from person to person but often include persistent or recurring pain in the pelvic region, discomfort in the genitals, urinary symptoms such as frequency or urgency, and sexual difficulties. The exact cause of CPPS is not well understood, but it may involve a combination of factors, including inflammation, muscle dysfunction, nerve sensitization, or psychological factors such as stress or anxiety.
Treatment Options for CPPS
The treatment of CPPS focuses on managing symptoms and improving quality of life. It often involves a multidisciplinary approach, including medication, physical therapy, lifestyle modifications, and psychological support. Medications such as alpha-blockers, anti-inflammatory drugs, or muscle relaxants may be prescribed to alleviate symptoms. Physical therapy techniques such as pelvic floor exercises or myofascial release may help relax muscles and relieve pain. Lifestyle modifications, including stress management techniques and dietary changes, may also be beneficial in managing symptoms. Psychological support, such as cognitive-behavioral therapy or counseling, can help individuals cope with the emotional impact of CPPS and develop effective pain management strategies.
Testing and Diagnosis of Prostate Disorders
Prostate-Specific Antigen (PSA) Test
The prostate-specific antigen (PSA) test is a blood test used to measure the levels of PSA in the bloodstream. PSA is a protein produced by the prostate gland, and elevated levels may indicate the presence of prostate disorders, including prostate cancer or prostatitis. However, it is important to note that an elevated PSA level does not necessarily indicate the presence of cancer, as other factors such as age, prostate size, or inflammation can also affect PSA levels. The PSA test is a valuable tool in prostate disorder screening and monitoring, but further diagnostic testing is often required to confirm a diagnosis.
Computed Tomography (CT) Scan
A computed tomography (CT) scan is a diagnostic imaging test that uses X-rays and computer processing to create detailed cross-sectional images of the body. It can provide information about the size, shape, and location of the prostate gland, as well as detect abnormalities such as tumors or cysts. A CT scan may be ordered if other tests suggest the presence of a prostate disorder or to evaluate the extent of a known condition.
Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging (MRI) is a non-invasive imaging test that uses magnetic fields and radio waves to produce detailed images of the body's internal structures. It can provide high-resolution images of the prostate gland and surrounding tissues, allowing for the detection and evaluation of abnormalities. MRI may be used in conjunction with other diagnostic tests to assess the presence and extent of prostate disorders or to guide treatment planning.
Biopsy of the Prostate
A prostate biopsy involves the removal of small tissue samples from the prostate gland for laboratory analysis. It is typically performed to confirm or rule out the presence of prostate cancer. During a biopsy, a thin needle is inserted into the prostate gland, guided by imaging techniques such as ultrasound. Several tissue samples are collected from different areas of the prostate and sent to a pathologist for examination under a microscope. The results of the biopsy can help determine the presence, extent, and aggressiveness of prostate cancer.
In conclusion, understanding the various prostate disorders and their associated risks, symptoms, and treatment options is essential for maintaining prostate health and overall well-being. If you experience any concerning symptoms or have any risk factors, it is important to consult with a healthcare professional for an accurate diagnosis and appropriate management. Regular screenings and early detection are crucial for improving outcomes and ensuring the best possible prognosis. Remember, taking care of your prostate health is taking care of yourself.

